- Courses
- GS Full Course 1 Year
- GS Full Course 2 Year
- GS Full Course 3 Year
- GS Full Course Till Selection
- Answer Alpha: Mains 2025 Mentorship
- MEP (Mains Enrichment Programme) Data, Facts
- Essay Target – 150+ Marks
- Online Program
- GS Recorded Course
- Polity
- Geography
- Economy
- Ancient, Medieval and Art & Culture AMAC
- Modern India, Post Independence & World History
- Environment
- Governance
- Science & Technology
- International Relations and Internal Security
- Disaster Management
- Ethics
- NCERT Current Affairs
- Indian Society and Social Issue
- NCERT- Science and Technology
- NCERT - Geography
- NCERT - Ancient History
- NCERT- World History
- NCERT Modern History
- CSAT
- 5 LAYERED ARJUNA Mentorship
- Public Administration Optional
- ABOUT US
- OUR TOPPERS
- TEST SERIES
- FREE STUDY MATERIAL
- VIDEOS
- CONTACT US
WHO Guidelines on Antimicrobial Resistance (AMR)
WHO Guidelines on Antimicrobial Resistance (AMR)
The World Health Organization (WHO) has recently published “Guidance on wastewater and solid waste management for manufacturing of antibiotics” to address the growing threat of Antimicrobial Resistance (AMR).
- This guidance aims to provide a scientific framework for controlling antibiotic resistance through effective waste management.
Key Highlights of the WHO Guidance:
About:
- Objective: To establish a scientific basis for setting targets and incorporating these into policies and regulations to combat antibiotic resistance.
- Nature: Non-binding but aims to promote consistency across policies, enhancing transparency and avoiding fragmented approaches.
Principles and Best Practices:
- Risk Management Plans: Recommends best practices for developing risk management plans, modeled on methods from food and water safety sectors.
- Audit and Transparency: Stresses the importance of regular audits and public transparency in antibiotic production and waste management.
- Progressive Implementation: Advocates for a stepwise approach to implementation, ensuring global protection and equitable access to quality antibiotics.
Target Audiences:
- Regulatory Bodies: National and regional authorities overseeing pharmaceutical manufacturing and waste management.
- Third-party Organisations: Entities responsible for audits and inspections of antibiotic production.
- Generic Substitution and Reimbursement Entities: Organisations handling decisions related to generic drugs and their reimbursement.
- Industrial Actors: Companies involved in antibiotic production.
- Waste Management Services: Entities managing disposal of antibiotic waste and wastewater.
Scope of the Guidance:
- Human Health-Based Targets: Aims to reduce antibiotic resistance risks.
- Ecotoxicological Risks: Addresses risks to aquatic ecosystems from antibiotic pollution.
- Coverage: Encompasses all stages of antibiotic production, from active pharmaceutical ingredients (APIs) to finished products and primary packaging.
- Waste Focus: Includes both liquid and solid waste, with a particular emphasis on liquid effluents and run-offs.
- Assessment Needs: Calls for separate risk assessments for sites producing multiple APIs or products.
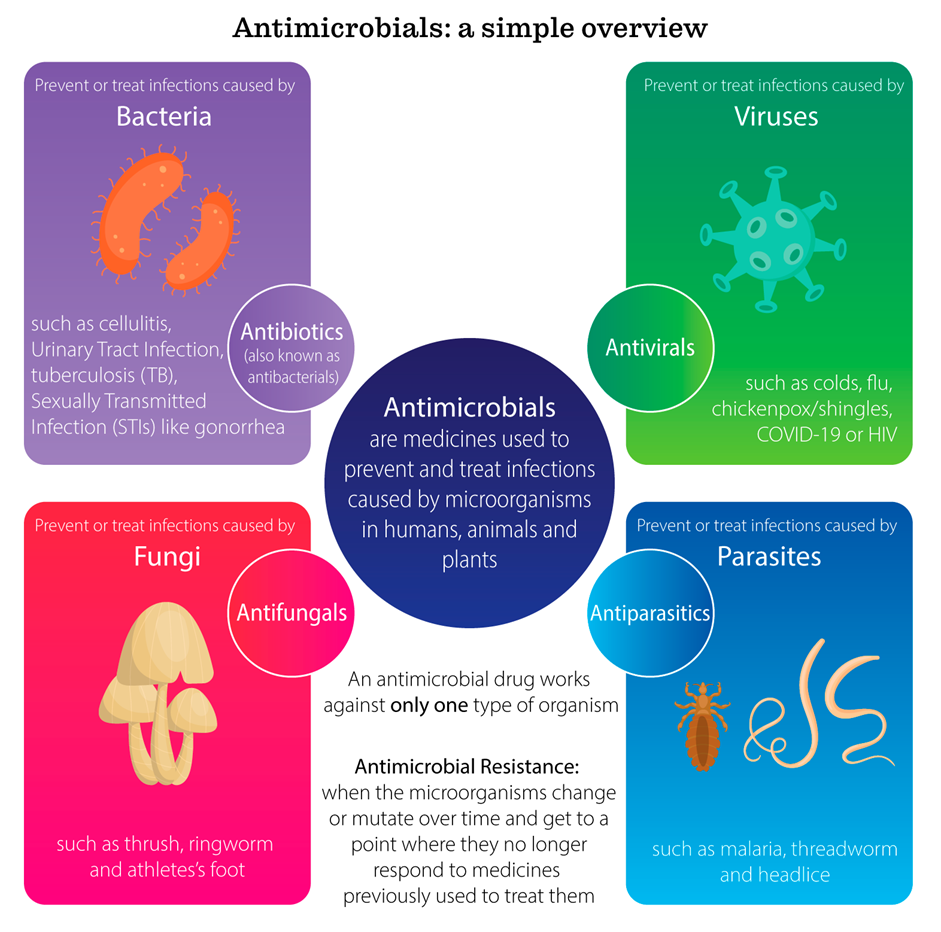
What is Antimicrobial Resistance (AMR)?
About AMR:
- Definition: AMR occurs when bacteria, viruses, fungi, or parasites no longer respond to antimicrobial medicines, making infections difficult or impossible to treat.
- Impact: Results in increased disease spread, severe illness, disability, and death.
Prevalence:
- Global Impact: Bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths.
Economic Cost:
- Healthcare Costs: Estimated at USD 1 trillion additional costs by 2050.
- GDP Losses: Projected losses of USD 1 trillion to USD 3.4 trillion per year by 2030.
Reasons for Increasing AMR:
- Individual Practices: Overuse of antibiotics for viral infections.
- Medical Practices: Use of broad-spectrum antibiotics leading to increased resistance.
- Diagnostic Challenges: Prescribing antibiotics based on symptoms rather than diagnostic tests.
- Pharmaceutical Manufacturing: Waste from antibiotic production contributing to the emergence of resistant bacteria.
Common Resistant Pathogens in India:
- E. Coli: Decreased susceptibility to carbapenems from 81.4% in 2017 to 62.7% in 2023.
- Klebsiella Pneumoniae: Reduced susceptibility to carbapenems from 58.5% to 35.6% and 48% to 37.6% between 2017 and 2023.
- Acinetobacter Baumannii: Highly resistant to even strong antibiotics, with no significant change in susceptibility.
How Can AMR be Tackled?
- Public Awareness Campaign: Launch long-term campaigns to reduce unnecessary antimicrobial prescriptions and educate the public.
- Improved Sanitation: Enhance sanitation practices, including regular handwashing and effective waste management.
- Reduce Unnecessary Use of Antimicrobials: Ensure appropriate use of antibiotics, reserving potent antibiotics for hospital use.
- Promote New and Rapid Diagnostics: Develop and use rapid diagnostic tests to reduce unnecessary antibiotic prescriptions.
- Vaccine Development and Alternative Therapies: Invest in new vaccines and alternative treatments such as phage therapy and probiotics to reduce antibiotic dependency.
- New Drug Development: Incentivize pharmaceutical companies to develop new antibiotics to address emerging resistance.
Conclusion:
The WHO's new guidance on managing antibiotic waste marks a crucial step in addressing the global challenge of Antimicrobial Resistance (AMR). By providing a framework for better waste management and promoting transparency and consistency in policies, the guidance aims to curb the rise of resistant pathogens. Given the severe health and economic impacts of AMR, this guidance is an important tool for regulators, industry, and other stakeholders. However, tackling AMR requires a multi-faceted approach, including public education, improved medical practices, and investment in new technologies and treatments. The combined efforts of all sectors will be essential to mitigate the growing threat of AMR and ensure effective management of antibiotic resources.