Why in the News?
- Antimicrobial resistance (AMR) is a growing public health threat in India, flagged by WHO as one of the top 10 global health risks, with projections of 10 million annual deaths worldwide by 2050.
- India’s position as the 2nd highest antibiotic consumer, with a 47% rise between 2010 and 2020, combined with over-the-counter access and poor sanitation which significantly accelerates resistance.
What is Antibiotic or Antimicrobial Resistance (ABR or AMR)?
Antibiotic resistance (ABR) occurs when bacteria evolve mechanisms to resist the effects of drugs that once killed them or inhibited their growth.
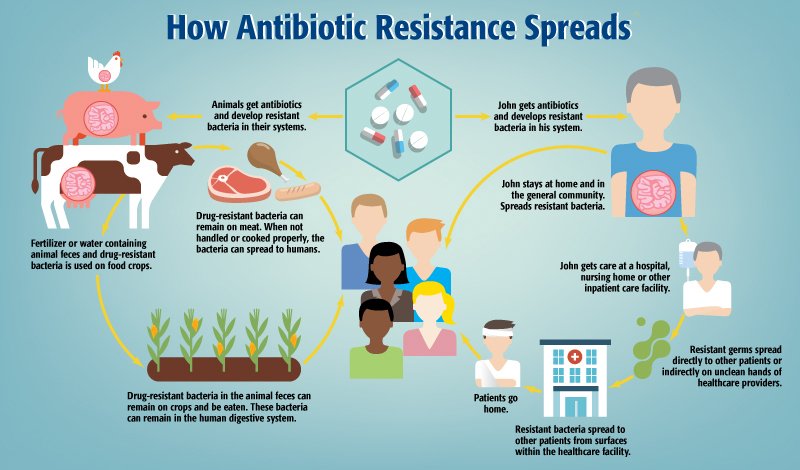
What are the causes of ABR?
- Human Misuse: Bacteria become resistant when antibiotics are misused (like Self-medication, incomplete antibiotic courses, and unnecessary prescription).
- Healthcare System Gaps: Inadequate diagnostics, poor infection control, and overcrowded hospitals facilitate the spread of resistant infections.
- Environmental Factors: Pharmaceutical waste, untreated sewage, and antibiotic residues in water bodies contribute to environmental resistance.
- Agricultural Practices: The use of antibiotics in agriculture, particularly as growth promoters, accelerates resistance development.
- Global Movement: International travel and trade facilitate the spread of resistant strains across borders.
Impact and Consequences
- Health: Increased mortality and morbidity due to treatment failures and prolonged illnesses.
- Economic: Higher healthcare costs, loss of productivity, and economic strain on families, especially in low-income settings.
- Social: Erosion of trust in medical systems and a rise in alternative medicine practices.
- Global: Threatens the effectiveness of surgeries, cancer treatments, and maternal care, undermining medical advancements.
- Examples: Some bacteria are becoming hard to treat, including:
- Tuberculosis (TB): Multi–Drug Resistant (MDR – resistant to some key drugs) and Extensively Drug Resistant (XDR – resistant to almost all drugs) strains.
- Gonorrhea, Pneumonia, and Urinary Tract Infections: Increasing resistance makes standard treatments less effective.
- Superbugs: Certain bacteria resist multiple antibiotics. The NDM-1 gene, discovered in India, makes some infections nearly untreatable with last-resort drugs like carbapenems.
Government Initiatives and Policy Framework
- National Action Plan on AMR (2017–2021): Launched by the Ministry of Health and Family Welfare (MoHFW), this plan focuses on surveillance, awareness, and regulation to combat AMR.
- Red Line Campaign: Introduced to mark antibiotics that are prescription- only, aiming to curb over-the-counter sales.
- AMR Surveillance Network: ICMR leads a national network monitoring resistance patterns across hospitals.
- FSSAI Regulations: The Food Safety and Standards Authority of India (FSSAI) has set norms to limit antibiotic use in food-producing animals.
- One Health Approach: Integrating human, animal, and environmental health to address AMR comprehensively.
Global Efforts and Best Practices
- WHO’s Global Action Plan on AMR: Provides a strategic framework for countries to combat AMR through surveillance, stewardship, and innovation.
- Tripartite Collaboration: WHO, FAO, and World Organisation for Animal Health (OIE) work together to coordinate global efforts against AMR.
- Antibiotic Stewardship Programs: Implemented in hospitals worldwide to optimize antibiotic use and reduce resistance.
- EU Regulations: The European Union has banned the use of antibiotics as growth promoters in livestock.
- Global Surveillance Systems: Systems like GLASS monitor resistance patterns and inform policy decisions.
Ethical and governance considerations in tackling ABR
- Access vs. Regulation: Balancing antibiotic availability with strict controls is vital. Over-regulation can hurt vulnerable groups; under-regulation fuels resistance.
- Equity in Treatment: Marginalized communities face limited access to effective care. Ethical governance must ensure no one is left behind.
- Pharmaceutical Responsibility: Companies must avoid overpromotion, ensure quality, support stewardship (responsible management and use of antibiotics to preserve their effectiveness.), and invest in new treatments.
- Civil Society’s Role: NGOs, media, and communities are key to spreading awareness, promoting hygiene, and supporting responsible antibiotic use.
Challenges and Way Forward
| Challenges | Way Forward |
| Weak enforcement & regulatory gaps: Prescription laws are not properly followed, and over-the-counter antibiotic sales still happen, leading to misuse. | Stronger rules & stewardship: Enforce prescription-only antibiotics, ban over-the-counter sales, and ensure hospitals adopt antibiotic stewardship programs. |
| Low awareness: People and healthcare workers do not fully understand antibiotic resistance (AMR). | Awareness campaigns: Educate the public and healthcare workers on the proper use of antibiotics. |
| Poor infrastructure: Not enough labs to test for resistant bacteria. | Improve diagnostics: Build more labs and make testing faster and easier. |
| Poor coordination: Health, agriculture, and environment departments do not work together. | One Health approach: Link human, animal, and environmental health policies. |
| Lack of research funding: Not enough money for new antibiotics or alternative treatments. | Promote research: Invest in developing new antibiotics and treatments. |
| Antibiotic use in livestock and environmental impact: Antibiotics in animals and pharmaceutical waste contribute to resistance. | Regulate use & environment: Control antibiotic use in farms and manage pharmaceutical waste to reduce environmental exposure and resistance spread. |
Conclusion
Antibiotic resistance is a pressing public health challenge that requires immediate and sustained action. A coordinated, multi-sectoral approach, integrating policy, education, and research, is essential to combat this threat. Future administrators must prioritize AMR in health governance to safeguard public health and ensure the efficacy of antibiotics for future generations.
| Ensure IAS Mains Question Q. “Antimicrobial resistance is a silent pandemic requiring urgent, coordinated action.” Analyse the challenges and suggest practical solutions for India. (250 words) |
| Ensure IAS Prelims Question Q. Consider the following statements regarding Antibiotic Resistance (ABR): 1. ABR occurs when bacteria evolve to survive exposure to antibiotics that previously killed them. 2. Over-the-counter antibiotic sales and misuse in humans and livestock are major drivers of ABR. 3. Antibiotic stewardship programs aim to completely eliminate the use of antibiotics in healthcare and agriculture. Which of the statements given above are correct? a) 1 and 2 only b) 2 and 3 only c) 1 and 3 only d) 1, 2 and 3 Answer: a) 1 and 2 only Explanation: Statement 1 is correct: ABR arises when bacteria develop mechanisms to survive antibiotics, making standard treatments ineffective. Statement 2 is correct: Misuse in humans (self-medication, incomplete courses) and overuse in livestock contribute significantly to ABR. Statement 3 is incorrect: Stewardship programs do not aim to eliminate antibiotics; they promote responsible and rational use to reduce resistance while ensuring access for patients in need. |
Also Read | |
| UPSC Foundation Course | UPSC Daily Current Affairs |
| UPSC Monthly Magazine | CSAT Foundation Course |
| Free MCQs for UPSC Prelims | UPSC Test Series |
| ENSURE IAS NOTES | Our Booklist |