Context
A new study published in Science Translational Medicine has mapped how rheumatoid arthritis (RA) evolves years before symptoms appear. The findings show that immune cells—T cells and B cells—become primed for autoimmune attack long before joint pain begins, opening the possibility of early diagnosis and early intervention to prevent joint damage.
What is Rheumatoid Arthritis?
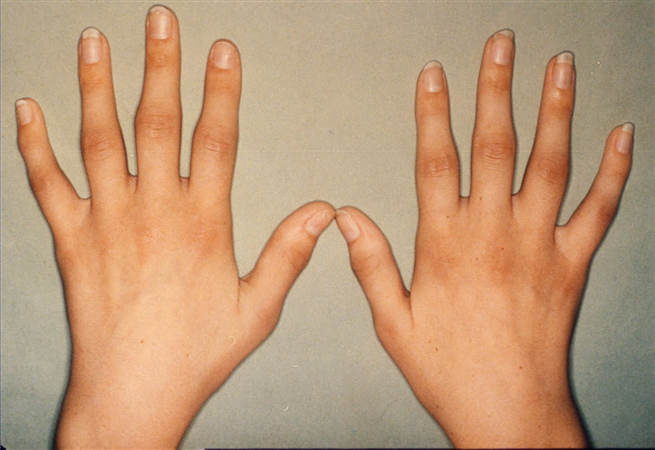
Rheumatoid arthritis is an autoimmune disease in which the body’s immune system mistakenly attacks its own joints.
Key features:
- Causes pain, stiffness, swelling, and progressive joint destruction
- Can also affect the lungs, heart, skin, eyes, and blood vessels
- More common in women (3x higher)
- Usually appears between ages 30–60
- Triggered by genetics, hormones, and environmental factors (smoking, infections)
The Global Burden of Disease Study projects an 80% rise in RA cases in the next 30 years, making early detection crucial.
Why is Early Detection Important?
- Most patients are diagnosed after significant immune damage has already occurred.
- By the time joint pain starts, immune disruption is already advanced.
- RA spreads beyond joints—causing fatigue, fever, depression, heart disease risk.
- Early-stage (preclinical) intervention could delay or prevent irreversible joint damage.
How the Disease Evolves Before Symptoms
- Silent Stage: Antibody Signals Appear Early
- Anticitrullinated protein antibodies (ACPAs) can appear 3–5 years before symptoms.
- People testing positive but without symptoms are called “at-risk individuals.”
- Only one-third of them progress to RA, making prediction difficult.
- Study Design
- Researchers followed:
- 45 ACPA-positive at-risk individuals
- 11 patients with early RA
- Researchers followed:
- 38 healthy individuals
- Over 18 months, 16 at-risk participants developed RA → called “converters.”
- Systemic Inflammation Already Active
- At-risk individuals—even those who never develop RA—already show:
- Higher inflammatory proteins (CXCL3, CXCL5, CXCL13)
- Early immune activation despite no symptoms
- This shows RA begins years before pain begins.
- At-risk individuals—even those who never develop RA—already show:
- Immune Cells Become “Primed”
- T cells:
- Naïve T cells show early activation signatures
- Epigenetic changes make NFAT–calcium signalling pathways more “open,” preparing them to overreact
- B cells:
- Begin switching towards inflammatory antibodies (IgG3)
- Release excess IL-6 and RANKL, molecules known to drive RA inflammation
- How “Converters” Differed
- Those who eventually developed RA showed:
- Growth of T cells that wrongly activate B cells
- B cells acquiring abnormal, autoimmune-supporting forms
- Those who eventually developed RA showed:
- T cells:
- Rise in inflammatory monocytes (TNF, IL-1B) once symptoms began
- Immune behaviours similar to those reversed by abatacept (a T-cell–targeting drug)
- Genetic Patterns
- Only small genetic differences were found, showing RA progression depends more on immune behaviour than genes alone.
Implications of the Study
- RA has a long preclinical phase with detectable immune changes.
- Early immune priming could become a biomarker for predicting who will develop RA.
- Treatments targeting early T-cell activation (e.g., abatacept) may prevent progression.
- Multi-omic data (genomic, transcriptomic, epigenetic profiles) may reshape early diagnosis.
Challenges and Way Forward
| Challenges | Way Forward |
| Difficult to identify at-risk individuals who will progress to RA. | Develop better biomarkers using multi-omic profiling and long-term cohort studies. |
| Risk of overtreatment if all ACPA-positive individuals are treated. | Use risk stratification tools to identify “high-risk converters.” |
| RA’s early immune changes are subtle and vary between individuals. | Improve sequencing, epigenetic mapping, and AI-based prediction models. |
| Current therapies begin only after clinical symptoms appear. | Shift to preclinical intervention, targeting early immune priming (e.g., T-cell co-stimulation blockers). |
| Multi-omic tests are expensive and not widely available. | Reduce costs through technology scaling; integrate early-detection tools in major hospitals. |
| Limited understanding of environmental triggers. | Strengthen research on smoking, microbiome, infections, and hormonal factors. |
Conclusion
The study shows that rheumatoid arthritis begins silently years before symptoms appear, with immune cells already “primed” for autoimmune attack. This fundamentally shifts our understanding of RA from a joint disease to a systemic, early-stage immune disorder. With advances in molecular mapping, early biomarkers, and targeted therapies like abatacept, the future of RA management may move toward prevention and early intervention, delaying or even avoiding the painful, disabling phase of the disease. These insights also create pathways to improve understanding and early detection of related autoimmune disorders such as lupus, type 1 diabetes, and multiple sclerosis.
| EnsureIAS Mains Question Q. Recent multi-omic research has revealed that immune changes associated with rheumatoid arthritis begin years before clinical symptoms appear. Discuss the significance of identifying this preclinical phase for disease prevention and early diagnosis. Highlight the challenges in translating these findings into clinical practice. (250 Words) |
| EnsureIAS Prelims Question Q. With reference to the preclinical phase of Rheumatoid Arthritis (RA), consider the following statements: 1. Anticitrullinated protein antibodies (ACPAs) can appear several years before joint pain begins. 2. All individuals who test positive for ACPAs eventually develop rheumatoid arthritis. 3. T cells and B cells show early activation and epigenetic priming even before symptoms appear. 4. Inflammatory proteins such as CXCL3, CXCL5, and CXCL13 increase only after clinical symptoms start. Which of the statements given above are correct? a) 1 and 3 only Answer: (a) 1 and 3 only Explanation Statement 1 is correct: ACPAs can appear 3–5 years before any symptoms begin, marking a silent preclinical stage in RA. Statement 2 is incorrect: Only one-third of ACPA-positive individuals progress to RA; the majority do not. Statement 3 is correct: The study found that T cells and B cells become “primed” with early activation signatures and epigenetic changes long before symptoms appear. Statement 4 is incorrect: Inflammatory proteins like CXCL3, CXCL5, and CXCL13 rise even in symptom-free at-risk individuals, showing that systemic inflammation occurs before clinical RA begins. |
Also Read | |
| UPSC Foundation Course | UPSC Daily Current Affairs |
| UPSC Monthly Magazine | CSAT Foundation Course |
| Free MCQs for UPSC Prelims | UPSC Test Series |
| Best IAS Coaching in Delhi | Our Booklist |